What is Cellulitis? An In-Depth Guide
Cellulitis is a common, potentially serious bacterial skin infection that affects millions of people worldwide. While it is often a manageable condition, it can become severe if left untreated, leading to complications that require prompt medical attention. This comprehensive guide will cover everything you need to know about cellulitis, including its causes, symptoms, diagnosis, treatment options, prevention strategies, and frequently asked questions.
1. Understanding Cellulitis
Definition
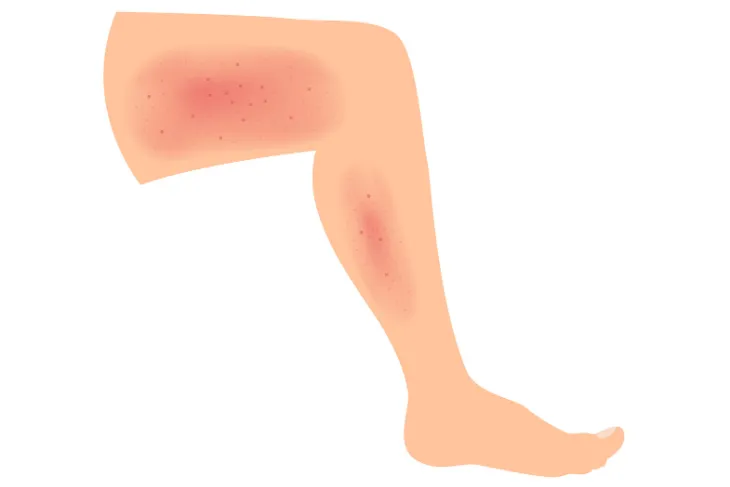
Cellulitis is a bacterial infection that affects the skin and the underlying tissue. It typically occurs when bacteria enter the skin through cuts, scrapes, or other breaks. The infection often presents as redness, swelling, warmth, and pain in the affected area, commonly on the legs, arms, or face. If left untreated, cellulitis can spread rapidly, potentially leading to life-threatening complications such as sepsis.
Common Misconceptions
Many people confuse cellulitis with other skin conditions, such as eczema or dermatitis, because of its similar appearance. Unlike these chronic conditions, cellulitis is an acute infection that requires immediate medical treatment.
2. Causes and Risk Factors
Bacteria Responsible for Cellulitis
The most common bacteria that cause cellulitis are:
- Streptococcus pyogenes (Group A Streptococcus): Often responsible for rapid-onset cellulitis.
- Staphylococcus aureus: Includes methicillin-resistant Staphylococcus aureus (MRSA), which is more challenging to treat.
These bacteria are part of the normal flora on the skin but can cause infections when they penetrate deeper layers.
Conditions that Increase Risk
Several factors can make individuals more susceptible to cellulitis:
- Skin Injuries: Cuts, scrapes, puncture wounds, or burns.
- Chronic Skin Conditions: Eczema, athlete’s foot, or psoriasis.
- Weakened Immune System: Due to conditions like diabetes, cancer, or HIV.
- Lymphedema: Swelling caused by lymphatic system blockages.
- Obesity: Increases the risk of skin breakdown.
- Surgical Procedures: Post-surgical wounds can act as entry points for bacteria.
3. Symptoms and Complications
Common Signs of Cellulitis
Symptoms of cellulitis usually develop quickly and can worsen without treatment:
- Redness: A spreading rash that is often warm to the touch.
- Swelling: The affected area becomes swollen and tender.
- Pain: Localized discomfort or pain.
- Fever and Chills: Indicating a systemic response to the infection.
- Blisters or Abscesses: In severe cases, the skin may develop blisters filled with fluid or pus.
When to Seek Medical Attention
Seek immediate medical care if you experience:
- Rapidly spreading redness or swelling.
- High fever or chills.
- Numbness or tingling in the affected area.
- Signs of infection near sensitive areas like the eyes or genitals.
Potential Complications
If untreated, cellulitis can lead to:
- Abscess Formation: Pockets of pus requiring drainage.
- Lymphangitis: Inflammation of lymphatic vessels.
- Sepsis: A life-threatening infection that spreads throughout the body.
- Recurrent Infections: Particularly in individuals with lymphedema or diabetes.
4. How Cellulitis is Diagnosed
Clinical Examination
Doctors typically diagnose cellulitis through a physical examination, noting the characteristic redness, warmth, and swelling. A thorough medical history helps identify underlying risk factors.
Diagnostic Tests
Additional tests may be needed in severe cases:
- Blood Tests: To detect systemic infection.
- Wound Culture: To identify the specific bacteria causing the infection.
- Imaging Studies: Ultrasound or MRI may be used to rule out deeper infections like abscesses.
5. Treatment Options
Antibiotics
Cellulitis is treated primarily with antibiotics:
- Oral Antibiotics: Prescribed for mild cases and typically taken for 5-10 days.
- Intravenous (IV) Antibiotics: Used for severe infections or when oral antibiotics are ineffective.
Common antibiotics include:
- Penicillin-based drugs (e.g., amoxicillin)
- Cephalexin
- Clindamycin
- Vancomycin (for MRSA)
Home Care and Supportive Measures
- Elevation: Keep the affected limb elevated to reduce swelling.
- Pain Relief: Use over-the-counter pain relievers like ibuprofen.
- Wound Care: Clean and bandage open wounds to prevent further infection.
Hospitalization and Advanced Treatments
Severe cases may require:
- IV Fluids and Medications: For systemic infections.
- Surgical Intervention: Drainage of abscesses or removal of necrotic tissue.
6. Prevention Strategies
Skin Care Best Practices
- Keep your skin moisturized to prevent cracking.
- Treat minor cuts or scrapes promptly with antiseptic and a clean bandage.
- Avoid walking barefoot in areas where injuries could occur.
Managing Underlying Conditions
- Maintain good blood sugar control if you have diabetes.
- Treat chronic skin conditions like eczema to reduce skin breaks.
- Use compression stockings if you have lymphedema.
7. Living with and Recovering from Cellulitis
Coping Mechanisms
- Follow your doctor’s instructions regarding medications and follow-up appointments.
- Be vigilant for early signs of recurrence.
Recurrence Prevention
- Address underlying risk factors.
- Practice good hygiene and skin care regularly.
8. Frequently Asked Questions About Cellulitis
Q: Is cellulitis contagious?
A: No, cellulitis itself is not contagious as it occurs when bacteria penetrate through your own skin.
Q: Can cellulitis recur?
A: Yes, especially if the underlying causes, such as lymphedema or diabetes, are not managed.
Q: What happens if cellulitis is left untreated?
A: Untreated cellulitis can lead to complications like sepsis, abscess formation, or necrotizing fasciitis.
Q: Can cellulitis be prevented?
A: Preventive measures such as proper wound care, hygiene, and managing chronic conditions can significantly reduce the risk.
9. Conclusion
Cellulitis is a serious but treatable skin infection that requires prompt medical attention. Understanding the causes, recognizing the symptoms, and seeking early treatment are essential for preventing complications. With proper care, most people recover fully from cellulitis. By adopting preventive measures and addressing underlying risk factors, the chances of recurrence can also be minimized.
If you suspect you have cellulitis, consult a healthcare provider promptly to ensure timely and effective treatment.
- Art
- Causes
- Crafts
- Dance
- Drinks
- Film
- Fitness
- Food
- Games
- Gardening
- Health
- Home
- Literature
- Music
- Networking
- Other
- Party
- Religion
- Shopping
- Sports
- Theater
- Wellness
